Joint Replacement
joint replacement surgery — also known as knee arthroplasty (ARTH-row-plas-tee) — can help relieve pain and restore function in severely diseased knee joints. The procedure involves cutting away damaged bone and cartilage from your thighbone, shinbone and kneecap and replacing it with an artificial joint (prosthesis) made of metal alloys, high-grade plastics and polymers.
In determining whether a knee replacement is right for you, an orthopedic surgeon assesses your knee’s range of motion, stability and strength. X-rays help determine the extent of damage.
a variety of knee replacement prostheses and surgical techniques, considering your age, weight, activity level, knee size and shape, and overall health.
The most common reason for knee replacement surgery is to relieve severe pain caused by osteoarthritis. People who need knee replacement surgery usually have problems walking, climbing stairs, and getting in and out of chairs. Some also have knee pain at rest.
Joint replacement surgery takes place in a hospital operating room while you are under anesthesia. During the procedure, the surgeon removes the damaged bone and cartilage, replacing them with prosthetic devices made of ceramic, metal or plastic.
Joint replacement surgery can be performed on hips, knees, shoulders, elbows, wrists and ankles. There are numerous approaches available to each of these procedures, and your doctor will discuss your options with you.
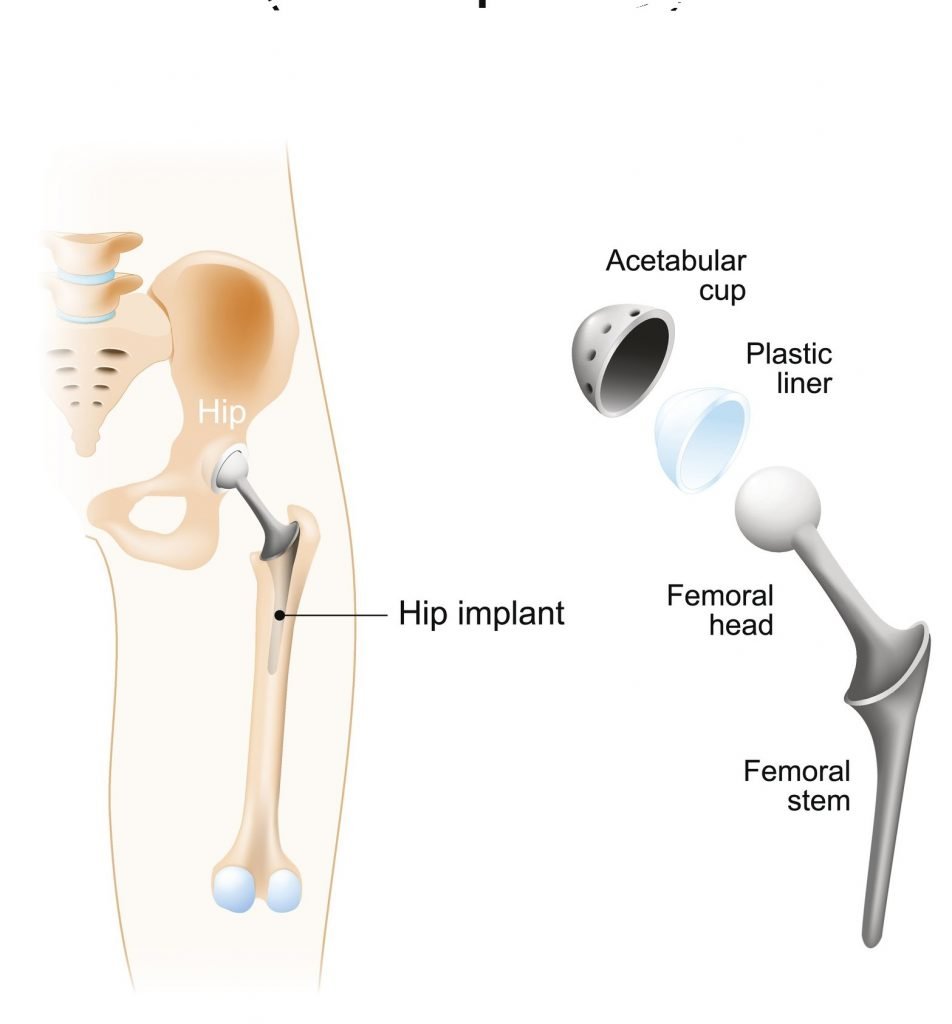
Total hip replacement surgery — After the damaged areas are removed from the femur and the pelvis, the femoral head (the ball) is replaced with a metal stem that holds a ball made of ceramic or metal, and a metal socket replaces the socket’s cartilage surface. A spacer made of ceramic, metal or plastic ensures the new ball and socket glide as they should.
Total knee replacement surgery — The cartilage and bone removed from the femur and tibia are replaced with metal components. A spacer, usually made of plastic, ensures the hinge joint of the knee bends smoothly.
Total shoulder replacement surgery — Damaged bone and cartilage are removed from the shoulder. Typically, the ball of the humerus is replaced with a metal ball on a stem, and a plastic socket is inserted in the scapula to make the new ball-and-socket joint.
Total elbow replacement surgery — A prosthetic elbow joint is made of two metal stems and a plastic or metal hinge. After the damaged bone and cartilage are removed, the metal stems are inserted into the humerus and ulna to allow the hinge to bend like a natural elbow.
Total wrist replacement — Damaged bone and cartilage are cleared away, and metal prosthetics are placed on the radial and carpal bones. A plastic spacer helps the wrist work properly.
Total ankle replacement — After the damage to the tibia and talus bones is removed, metal prosthetics are added to the bone surfaces with a plastic spacer inserted between the metal.
Knee and hip replacements are two of the most commonly performed elective operations. For the majority of patients, joint replacement surgery relieves pain and helps them to live fuller, more active lives.
No surgical procedure is without risks, however. A small percentage of patients undergoing hip or knee replacement (roughly about 1 in 100) may develop an infection after the operation.
Joint replacement infections may occur in the wound or deep around the artificial implants. An infection may develop during your hospital stay or after you go home. Joint replacement infections can even occur years after your surgery.
This article discusses why joint replacements may become infected, the signs and symptoms of infection, treatment for infections, and preventing infections.
Before major surgery is performed, a complete pre-anaesthetic work-up is required. In elderly people this usually would include ECG, urine tests, hematology and blood tests. Cross match of blood is routine also, as a high percentage of people receive a blood transfusion. Pre-operative planning requires accurate Xrays of the affected joint, implant design selecting and size-matching to the xray images (a process known as templating).
A few days’ hospitalization is followed by several weeks of protected function, healing and rehabilitation. This may then be followed by several months of slow improvement in strength and endurance.
Early mobilisation of the person is thought to be the key to reducing the chances of complications such as venous thromboembolism and Pneumonia. Modern practice is to mobilize people as soon as possible and ambulate with walking aids when tolerated. Depending on the joint involved and the pre-op status of the person, the time of hospitalization varies from 1 day to 2 weeks, with the average being 4–7 days in most regions.
Physiotherapy is used extensively to help people recover function after joint replacement surgery. A graded exercise programme is needed initially, as the person’s muscles take time to heal after the surgery; exercises for range of motion of the joints and ambulation should not be strenuous. Later when the muscles have healed, the aim of exercise expands to include strengthening and recovery of function.



